Tetanus Poisoning
What is Tetanus Poisoning?
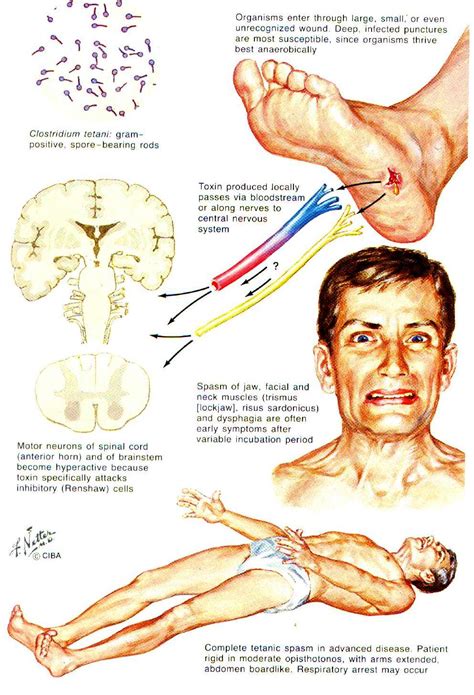
Tetanus poisoning, also known as lockjaw, is a serious bacterial infection caused by the bacteria Clostridium tetani. This bacterium is commonly found in soil, dust, and animal feces. Tetanus poisoning occurs when the bacteria enter the body through a wound or injury, usually a deep puncture wound.
Once inside the body, the bacteria release a powerful toxin called tetanospasmin. This toxin affects the nervous system by blocking the release of certain neurotransmitters that control muscle movement. As a result, muscles become stiff and spasms can occur. These spasms mainly affect the muscles in the jaw and neck, hence the term “lockjaw.”
It’s important to note that tetanus is not contagious and cannot be spread from person to person. However, it can be a life-threatening condition if not treated promptly. Tetanus is more commonly found in developing countries with limited access to healthcare and vaccination programs.
Causes of Tetanus Poisoning
Tetanus poisoning, also known as lockjaw, is a serious bacterial infection caused by the bacterium Clostridium tetani. This bacterium is commonly found in soil, dust, and manure. When it enters the body through a wound, it produces a toxin called tetanospasmin that affects the nervous system. While tetanus can be prevented through vaccination, understanding the causes of tetanus poisoning can help individuals take necessary precautions to avoid this potentially life-threatening condition.
There are several common causes of tetanus poisoning:
- Wounds: Tetanus bacteria can enter the body through any puncture wound, especially if it is deep and dirty. It is crucial to thoroughly clean and disinfect wounds to minimize the risk of infection.
- Contaminated Objects: Using tools or equipment that are contaminated with the tetanus bacterium can lead to infection. This can occur when working in gardens, farms, or construction sites, where the bacteria are more likely to be present.
- Animal Bites: Certain animal bites, such as those from dogs, cats, or rodents, can introduce tetanus bacteria into the bloodstream. It is important to seek medical attention promptly if bitten by an animal.
In addition to these causes, individuals who have not received a tetanus vaccine or have not kept their vaccination up to date are at a higher risk of tetanus poisoning. While anyone can develop tetanus, certain factors may increase the susceptibility to the infection, such as advanced age, diabetes, or a compromised immune system.
It is crucial to understand the causes of tetanus poisoning to minimize the risk of infection. By practicing proper wound care, avoiding contact with contaminated objects, and ensuring vaccination against tetanus, individuals can significantly reduce the likelihood of developing this serious condition.
Symptoms and Diagnosis of Tetanus Poisoning
Tetanus poisoning, also known as lockjaw, is a serious bacterial infection caused by Clostridium tetani. This bacteria enters the body through cuts, wounds, or puncture injuries, and releases a toxin that affects the nerves and muscles. While tetanus is relatively rare in developed countries due to widespread vaccination, it can still occur, especially in cases of inadequate immunization or unvaccinated individuals. In this blog post, we will delve into the symptoms and diagnosis of tetanus poisoning.
The incubation period for tetanus can range from a few days to several weeks, typically averaging around 8 days. The initial symptoms often include muscle stiffness and spasms, commonly starting with the muscles of the jaw and neck. This is why tetanus is often referred to as “lockjaw.” These spasms can make it difficult to open the mouth, swallow, or even breathe properly.
Furthermore, tetanus can cause muscle stiffness and spasms in other areas of the body, such as the abdomen, back, and limbs. These spasms are usually painful and can be triggered by external stimuli like noise or touch. In severe cases, muscle spasms can become so intense that they lead to fractures or muscle tears.
Diagnosing tetanus poisoning can be challenging, as there are no specific laboratory tests to confirm the infection. Diagnosis is primarily based on clinical symptoms and history of exposure to the bacteria. The healthcare provider will assess the individual’s symptoms, conduct a physical examination to look for muscle stiffness and spasms, and inquire about recent injuries or wounds.
It is crucial to mention any potential sources of infection, such as an unclean wound or an environment with a high risk of tetanus spores, as this information can aid in the diagnosis. Additionally, a doctor may use imaging tests, like an X-ray, to identify any fractures or muscle damage caused by the spasms. This can further support the diagnosis of tetanus poisoning.
- Symptoms of tetanus poisoning:
- Muscle stiffness and spasms, starting with the jaw and neck
- Painful muscle spasms in the abdomen, back, and limbs
- Difficulty swallowing and breathing
- High fever and sweating
- Increased heart rate and blood pressure
- Generalized body weakness and fatigue
While the symptoms mentioned above can strongly suggest tetanus poisoning, it is essential to rule out other conditions that may cause similar symptoms. These conditions can include other bacterial infections, muscle disorders, or neurological diseases. Therefore, a comprehensive evaluation is necessary to make an accurate diagnosis.
| Diagnostic criteria for tetanus poisoning: | Exclusion criteria: |
|---|---|
| Presence of characteristic symptoms and signs | Other diagnosable causes for symptoms |
| History of exposure to tetanus spores or inadequate immunization | Normal laboratory test results |
| Supportive imaging findings (e.g., fractures, muscle damage) | Alternative diagnosis confirmed by additional tests |
Overall, identifying the symptoms and diagnosing tetanus poisoning requires a thorough assessment of the individual’s clinical presentation, medical history, and potential exposure to the bacteria. Timely recognition of symptoms is crucial for prompt treatment and management of tetanus poisoning, as the infection can be life-threatening if left untreated.
Treatment Options for Tetanus Poisoning
Tetanus poisoning, also known as lockjaw, is a serious condition caused by the bacterium Clostridium tetani. This bacteria can enter the body through a wound or cut, and produce a toxin that affects the nervous system. The toxin causes muscle stiffness and spasms, leading to difficulty in breathing and swallowing. If left untreated, tetanus poisoning can be life-threatening. Therefore, prompt and appropriate treatment options are crucial in managing this condition.
When it comes to treating tetanus poisoning, there are several options available depending on the severity of the condition. The primary goal of treatment is to neutralize the toxin, control muscle spasms, and prevent complications. Let’s explore some of the treatment options:
1. Administration of tetanus immune globulin (TIG): TIG is a medication that contains antibodies to the tetanus toxin. It is given to neutralize the circulating toxin in the body. TIG is typically administered as a single dose after cleaning and preparing the wound.
2. Tetanus vaccine: If an individual has not received a tetanus vaccine in the past five years, a tetanus toxoid vaccine is administered. This helps boost the body’s immune response against the bacterium and prevents future infections.
3. Wound care: Proper wound care is essential in the treatment of tetanus poisoning. The wound should be thoroughly cleaned, and any foreign objects or debris should be removed. In some cases, surgical intervention may be required to clean and repair the wound.
4. Medications to control muscle spasms: Muscle spasms are a hallmark symptom of tetanus poisoning. Medications such as muscle relaxants and sedatives may be prescribed to alleviate these spasms and prevent further complications.
5. Supportive care: During treatment, it is important to provide supportive care to the patient. This may include monitoring vital signs, ensuring proper hydration, and addressing any complications that may arise.
It is imperative to seek immediate medical attention if there is a suspicion of tetanus poisoning. Early diagnosis and initiation of treatment can significantly improve the outcome and prevent severe complications. Remember, prevention is always better than cure. Ensuring proper wound care, staying up to date with tetanus vaccinations, and taking necessary precautions can help prevent tetanus poisoning altogether.
Prevention of Tetanus Poisoning
Tetanus, also known as lockjaw, is a serious bacterial infection that affects the muscles and nerves. It is caused by the bacterium Clostridium tetani, which is commonly found in soil, dust, and animal feces. Tetanus can enter the body through a wound or cut, and if left untreated, it can lead to life-threatening complications. Therefore, prevention of tetanus poisoning is crucial to ensure the health and safety of individuals.
1. Keep your vaccinations up to date: One of the most effective ways to prevent tetanus poisoning is through vaccination. The tetanus vaccine, usually given in combination with diphtheria and pertussis vaccines, is recommended for both children and adults. It is important to follow the recommended vaccination schedule and receive booster shots every 10 years to maintain immunity against tetanus.
2. Practice proper wound care: Tetanus bacteria can enter the body through cuts, puncture wounds, burns, or any skin injury. To prevent infection, it is essential to clean wounds with soap and water thoroughly. Applying an antiseptic solution can further reduce the risk of tetanus. If the wound is deep or you are unsure about its cleanliness, seek medical attention to ensure proper care and prevention of tetanus.
3. Be cautious with outdoor activities: Since tetanus bacteria are commonly found in soil, prevention measures should be taken during outdoor activities. If you are gardening, handling soil, or working in areas where there may be exposure to dirt, wearing protective gloves can minimize the risk of tetanus infection. Additionally, it is advisable to wear appropriate footwear to prevent cuts or puncture wounds from sharp objects.
- 4. Maintain good hygiene practices: Practicing good hygiene can also play a role in preventing tetanus poisoning. It is important to wash your hands thoroughly with soap and water before eating or handling food, especially if you have been in contact with soil or dirty surfaces.
- 5. Educate yourself and others: Spreading awareness and knowledge about tetanus and its prevention is crucial in minimizing the risk of tetanus poisoning. Educate yourself and others about the importance of tetanus vaccination, wound care, and hygiene practices. This can help ensure a safer environment for everyone.
| Risk factors for tetanus | Preventive measures |
|---|---|
| Poor vaccination history | Keep vaccinations up to date |
| Unprotected wounds or cuts | Practice proper wound care |
| Exposure to contaminated soil | Be cautious with outdoor activities and wear protective gloves |
| Insufficient hygiene practices | Maintain good hygiene practices |
| Lack of awareness | Educate yourself and others about tetanus prevention |
By following these preventive measures, you can significantly reduce the risk of tetanus poisoning. Remember, prevention is always better than cure when it comes to potentially life-threatening infections like tetanus.
Frequently Asked Questions
1. What is tetanus poisoning?
Tetanus poisoning is a bacterial infection caused by the bacteria Clostridium tetani. It affects the nervous system and can cause severe muscle stiffness and spasms.
2. What are the causes of tetanus poisoning?
The bacteria Clostridium tetani is commonly found in soil, dust, and animal feces. Tetanus can occur when the bacteria enters the body through a wound or cut, especially if the wound is deep and exposed to dirt or contaminated objects.
3. What are the symptoms and how is tetanus poisoning diagnosed?
The symptoms of tetanus poisoning include muscle stiffness and spasms, particularly in the jaw muscles (lockjaw), neck, and abdomen. Other symptoms may include difficulty swallowing, fever, sweating, and high blood pressure. Diagnosis is usually based on clinical symptoms and history of a recent wound or injury.
4. What are the treatment options for tetanus poisoning?
Treatment for tetanus poisoning typically involves administering a tetanus antitoxin to neutralize the toxin produced by the bacteria. Antibiotics may also be prescribed to fight the infection. In severe cases, supportive care such as respiratory assistance and muscle relaxants may be needed.
5. How can tetanus poisoning be prevented?
Tetanus can be prevented through vaccination. The tetanus vaccine is usually given as part of the routine childhood immunization schedule, and booster doses are recommended every 10 years for adults. It is also important to keep wounds clean and properly treated to minimize the risk of tetanus infection.
6. Can tetanus poisoning be fatal?
Yes, tetanus poisoning can be fatal, especially if not treated promptly and appropriately. The spasms and stiffness associated with tetanus can lead to breathing difficulties and other complications.
7. Is tetanus poisoning contagious?
No, tetanus is not contagious. It cannot be transmitted from person to person. The bacteria that cause tetanus are commonly found in the environment and enter the body through wounds or cuts.